Autoimmune Diseases
Table of Contents
Autoimmune diseases are conditions in which your immune system mistakenly damages healthy cells in your body. Types include Hashimoto’s Thyroiditis, Rheumatoid Arthritis, Crohn’s disease, and Psoriasis.
Your immune system usually protects you from diseases and infections. When it senses these pathogens or toxigens, it creates specific cells to target foreign cells.
Usually, your immune system can tell the difference between foreign cells and your own cells. But if you have an autoimmune disease, your immune system mistakes parts of your body, such as your organs, joints, and skin, as foreign. It releases proteins called autoantibodies that attack healthy cells.
Some autoimmune diseases target only one organ. Hashimoto’s Thyroiditis damages your thyroid. Other conditions, such as systemic lupus erythematosus, or lupus, can affect your whole body. In both situations, many aspects of your body’s functions can be disrupted. The most difficult part is finding the right help to overcome from an autoimmune disease. Dr. Trish Leigh knows, from personal experience, how important this is.
Below, we provide an overview of some of the most common autoimmune diseases.
What Can Cause Autoimmune Disease?
Science shows that many autoimmune diseases are related to autonomic nervous system (ANS) dysfunction. This causes the immune system to misfire. Some people are more likely to get an autoimmune disease than others due to certain risk factors, such as:
- Your sex: Women between the ages of 15 and 44 are more likely to get an autoimmune disease than men.
- Your family history: You may be more likely to develop autoimmune diseases due to your hereditary disposition, although environmental factors are highly contributing too.
- Environmental factors: Exposure to mold, toxins, sunlight, mercury, chemicals like solvents or those used in agriculture, cigarette smoke, or certain bacterial and viral infections, including COVID-19, may increase your risk of autoimmune disease.
- Ethnicity: Some autoimmune diseases are more common in people in certain groups. For example, white people from Europe and the United States may be more likely to develop autoimmune muscle disease, while lupus tends to occur more in people who are African American, Hispanic, or Latino.
- Nutrition: Your diet and nutrients may impact the risk and severity of autoimmune disease.
- Other health conditions: Certain health conditions, including chronic stress, obesity, and other autoimmune diseases, may make you more likely to develop an autoimmune disease.
Brain Dysfunction and Autoimmune Disorders
Studies indicate that the Autonomic Nervous System (ANS) regulates both innate and adaptive immunity through the sympathetic (fight or flight) and parasympathetic (rest and digest) branches, and an imbalance in this system can determine an altered inflammatory response, as typically observed in chronic conditions such as systemic autoimmune diseases.
Autoimmune diseases trigger the body into a red alert state as it is in a heightened state of hyperarousal. This “wired” state increases anxiety and stress responses. Coupled with the brain’s excessive fast speed, hypoarousal results in the nervous system becoming overwhelmed, exhausted, or tired. The chronic, wired, and tired state contributes to and perpetuates autoimmune responses. Many professionals are not aware of this relationship, making it difficult for patients to find help for autoimmune diseases.
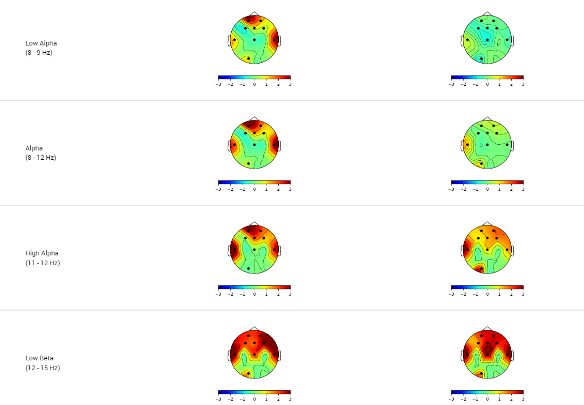
This brain performance pattern can be determined and visualized on a specialized brain scan called a qEEG, quantitative electroencephalogram. Dr. Trish Leigh is a global leader in providing qEEG brain scans using at-home technology. Having your brain performance evaluated is easier and more cost-effective now than ever. This state-of-the-art technology can indicate the areas and degree of brain dysfunction that may contribute to autoimmune diseases through ANS brain dysfunction. The qEEG Brain Map below exemplifies autoimmune dysfunction, as indicated by the red colors.
See what is included below.
What are the Common Symptoms of an Autoimmune Disease?
Different autoimmune diseases may have similar early symptoms. These can include:
- Fatigue
- Dizziness or Lightheadedness
- Trouble Concentrating
- Hair Loss
- Skin Rash
- Low-Grade Fever
- Muscle Aches
- Joint pain and Swelling
- Swollen Glands
- Abdominal Pain or Digestive Issues
With some autoimmune diseases, including psoriasis or rheumatoid arthritis (RA), symptoms may come and go. A period of symptoms is called a flare-up. A period when the symptoms go away is called remission. Other autoimmune diseases can lead to a host of other health challenges, such as Mast Cell Activation Syndrome (MCAS), which leads to Multiple Chemical Sensitivities (MCS), Chronic Inflammatory Response Syndrome (CIR), and more.
Individual autoimmune diseases can also have unique symptoms depending on the body systems affected. For example, you may experience dry eyes and mouth with Sjogren’s disease. Inflammatory bowel disease (IBD) may cause bloating and diarrhea. Symptoms can vary depending on what areas of your brain and body are affected.
What are the Most Common Autoimmune Diseases?
Researchers have identified more than 100 autoimmune diseases. Here are 10 more common ones.
Mast Cell Activation Syndrome (MCAS) is the most common form of systemic Mast Cell Disease and is known to cause Dysautonomia in some people. Activation of high levels of mast cell mediators in the body in response to exposure to environmental triggers. Dr. Trish Leigh is a highly trained professional who knows how to provide fast, effective autoimmune disease help because she suffered from MCAS for years. If you meet her, ask her about the Turkish carpet incident. It was not pretty.
MCAS can be triggered by food, chemicals, toxins, mold, air quality, and other environmental exposures leading to:
- Multiple Chemical Sensitivities
- Migraine Headaches
- Nerves: pain
- Skin: itching, flushing, hives, sweating, swelling, rash.
- Eyes: irritation, itching, watering.
- Nose: itching, running.
- Mouth and Throat: itching, swelling in your tongue or lips, swelling in your throat.
- Lungs: trouble breathing, wheezing.
- Heart and Blood Vessels: low blood pressure, rapid heart rate.
In RA, your immune system attacks the joints. This causes symptoms affecting the joints such as:
- Swelling
- Warmth
- Soreness
- Stiffness
While RA affects people as they get older, it can also start as early as your 30s. RA may be experienced in conjunction with other conditions such as Toxic Mold Poisoning. A related condition, juvenile idiopathic arthritis, can start in childhood.
Skin cells grow and then shed when they’re no longer needed. Psoriasis causes skin cells to multiply too quickly. The extra cells build up and form inflamed patches. On lighter skin tones, patches may appear red with silver-white scales of plaque. On darker skin tones, psoriasis may appear purplish or dark brown with gray scales.
Up to 30% of people with psoriasis also develop psoriatic arthritis. This can cause joint symptoms that include:
- Swelling
- Stiffness
- Pain
Multiple sclerosis (MS) damages the protective coating surrounding nerve cells (myelin sheath) in your central nervous system. Damage to the myelin sheath slows the transmission speed of messages between your brain and spinal cord to and from the rest of your body.
This damage can lead to:
- Numbness
- Weakness
- Balance issues
- Trouble walking
Different forms of MS progress at different rates. Difficulties with walking are one of the most common mobility issues with MS.
Although lupus was first described as a skin disease because of the rash it commonly produces, the most common systemic form, actually affects many organs. This can include you:
- Joints
- Kidneys
- Brain
- Heart
IBD describes conditions that cause inflammation in the lining of the intestinal wall. Each type of IBD affects a different part of your gastrointestinal (GI) tract although all involve chronic inflammation that can be related to ANS dysfunction.
Crohn’s disease can inflame any part of your GI tract, from the mouth to the anus.
Ulcerative colitis affects the lining of the large intestine (colon) and rectum.
Common symptoms of IBD can include:
- Diarrhea
- Abdominal pain
- Bleeding ulcers
Graves’ disease involves dysregulated signaling from the pituitary gland in your brain communicating with the thyroid gland in your neck, causing it to produce too much of its hormones. Thyroid hormones control the body’s energy usage, known as metabolism.
Having too much of these hormones revs up your body’s activities, causing symptoms that may include:
- Rapid heart rate (tachycardia)
- Heat intolerance
- Unintentional weight loss
- Swelling of the thyroid gland (goiter)
- Some people with Graves’ disease may also experience symptoms affecting the skin (Graves’ dermopathy) or eyes (Graves’ ophthalmopathy)
This condition dysregulates the glands that provide lubrication to your eyes and mouth.
The hallmark symptoms of Sjögren’s disease are dry eyes and dry mouth, but it may also affect your joints or skin. Burning Mouth Syndrome, which is identified as an ANS dysfunction, can be related to Sjogrens. Many times patients are told that there is no cause and no way to help this autoimmune disease. Dr. Trish Leigh can help you learn what you need to heal your autoimmune condition.
In Hashimoto’s thyroiditis, thyroid hormone production slows to a deficiency. Also, studies show that the brain slows down and that the sleep cycle is disrupted. Common symptoms of Hashimoto’s thyroiditis can include:
- Weight gain
- Sensitivity to cold
- Fatigue
- Hair loss
- Swelling of the thyroid (goiter)
Addison’s disease affects the adrenal glands, which produce the hormones cortisol and aldosterone as well as androgen hormones. Too little cortisol can affect how your body uses and stores carbohydrates and sugar (glucose). Too little aldosterone can lead to sodium loss and excess potassium in your bloodstream. ANS dysfunction contributes to cortisol production deficiencies.
Common symptoms of Addison’s disease can include:
- Weakness
- Fatigue
- Weight loss
- Low blood sugar
What are the 5 Common Symptoms of an Autoimmune Disorder?
- Fatigue
- Dizziness
- Low-grade fever
- Muscle aches
- Swelling
What are the 5 Most Common Autoimmune Disorders?
Psoriatic Arthritis
Rheumatoid Arthritis
Connective Tissue Diseases
Multiple Sclerosis
Autoimmune Thyroid Diseases
Such as Hashimoto’s, Celiac Disease, and Inflammatory Bowel Disease.
Summary
The symptoms of autoimmune diseases often overlap, complicating diagnoses.
As a survivor who has triumphed over most of these autoimmune disorders, Dr. Trish Leigh knows how to help individuals suffering from autoimmune disorders.
Although blood tests can help doctors diagnose these conditions, qEEG Brain Mapping can identify the underlying dysfunctional brain patterns that contribute to autoimmune disorders due to ANS dysfunction. After identification of the underlying contributing neurological dysregulation, neuromodulation techniques, including Neurofeedback Coaching, can be implemented at home to calm the overactive immune response and bring down inflammation in the body.
Autoimmune diseases do not have to persist for a lifetime with advances in technology and neuroscience.